HCV micro-elimination in PWUD
The autonomous community of the Balearic Islands (Mallorca, Menorca and Ibiza) delivered a micro-elimination project seeking to identify, link to care, and monitor re-infection through a new model of care aimed at people who inject drugs (PWID).
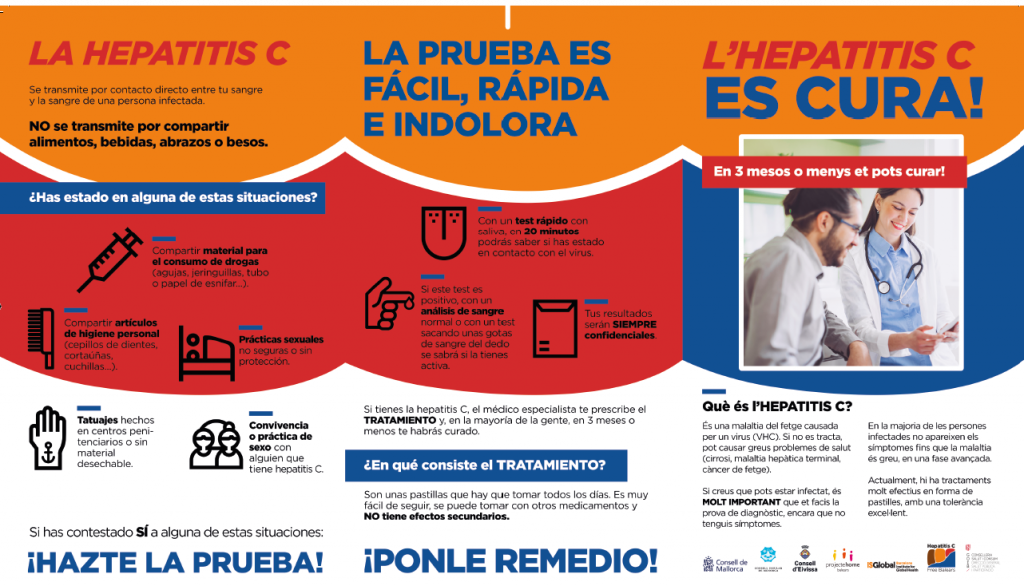
The initiative embraced point-of-care rapid diagnostic tests (OraQuick®) and dried blood spot testing and, when appropriate, linked patients to decentralised treatment in line with national treatment guidelines. The project offers a simplified care model for PWID who are treated in addiction service centres, mobile methadone units or in prison settings.
Who?
The project was operated by the Barcelona Institute for Global Health (ISGlobal) and the Health Service of the Balearic Islands (IBSalut) with the support of regional addiction services centres (i.e., Consell de Mallorca (IMAS), Consell de Menorca, Consell d’Eivissa, Projecte Home, Creu Roja Balears), the prison centre Centre Penitenciari de Mallorca, and Public Hospitals of the Balearic Islands (i.e., Hospital Universitari Son Llàtzer, Hospital Universitari Son Espases, Hospital Comarcal d’Inca, Hospital Comarcal de Manacor, Hospital Can Misses and Hospital Mateu Orfila).
Why?
Direct-acting antiviral (DAA) therapy can cure more than 95% of people with HCV, but there is insufficient HCV screening and, consequently, underuse of these therapies around the world. This is also the case for many of Spain’s 17 autonomous communities (regions) despite the country’s national viral hepatitis strategy (in place since May 2015) and unrestricted access to DAA treatment since June 2017.
The autonomous community of the Balearic Islands has a total population of 1.13 million with an estimated 1,400 individuals living with an untreated HCV infection. Up to 1,120 of this population are PWID, a key risk group for HCV and contributor to increasing infection rates. The size of the Balearic Islands and the proximity between the three major islands makes this an ideal setting for such a project.
Health system barriers deter many HCV-infected PWID from receiving care in traditional healtcare settings (i.e., hospitals), creating a need to engage them in other settings. Research has shown that PWID are receptive to receiving HCV screening at addiction service centres, but a lack of resources, infrastructure, and expertise often prevent such centres from offering HCV screening. Even when screening takes place, HCV-infected PWID typically present late for care or are lost to follow-up before undergoing confirmatory HCV testing or receiving additional care.
Creating new care pathways or leveraging existing ones to scale up the currently limited and dispersed treatment services for PWID, is essential to eliminating hepatitis C in this risk group. Such projects thus make a significant contribution to achieve the World Health Organization (WHO) goal of viral hepatitis elimination as a public health threat by 2030.
How?
The project followed 5 key steps:
- Obtain approval from community health authorities
- Obtain support from the centres and organisations involved in addiction control at regional level
- Obtain support from relevant healthcare professionals in the community, namely hepatologists, microbiologists and pharmacists from public hospitals
- Obtain authorisation to access the patient information charts of those participating in the project.
- Organise training on HCV and the project protocols for personnel working at the centres and organisations involved in addiction control services.
The study had several innovative features including HCV testing and linkage to care in addiction service centres (Metabús, Projecte Home and the governmental addiction service centres (UCAs)), alongside the delivery of prescribed DAAs by the study coordinator. Dried blood spot testing was used to simplify the care pathway at all sites, including for the monitoring for reinfection. Testing and linkage to care was provided for PWID who have entered the penitentiary system and to those who are released on bail. Tele-prescription of HCV treatment, based on HCV RNA results, was offered without requiring a face-to-face patient consultation.
Outcomes
To date, 877 patients have been recruited. Of those, 279 (32%) were anti-HCV antibodies positive and 110 (13%) were HCV-RNA positive. Of those who were HCV-RNA positive, 90 (82%) have initiated treatment and 66 (60%) have finished treatment. SVR12 monitoring tests were performed in 33 (50%) of those who finished treatment and 97% (n=32) of them showed undetectable HCV-RNA.
Learnings / Recommendations
The support of local authorities and the involvement of multidisciplinary teams are essential for success. Furthermore, good communication between hospital professionals and staff at addiction control centres, common action protocols, and a decentralised approach are key to promoting elimination of hepatitis C amongst vulnerable populations.
FUNDING
Private funding.
Contact
Jeffrey Lazarus, ISGlobal
jeffrey.lazarus@isglobal.org